Santa Dog's a Jesus Fetus
Santa Dog's a Jesus Fetus Santa Dog's a Jesus Fetus Has no presents, Has no presence In the future... ...In the future
I started blogging mid March 2012 and until now, made 18 posts. As we approach Christmas and the end of the year, here are my Top 5 in terms of views
Santa Dog by the Residents (my favourite xmas song)
Number 5: Whats Your Poison - LSD vs Alcohol At number 5 was my very first post on the meta-analysis by Krebs & Johansen suggesting using LSD as a treatment for alcoholism. The study attrated a lot of media attention and the following striking comment from Prof David Nutt that: "Overall there is a big effect, show me another treatment with results as good; we've missed a trick here…This is probably as good as anything we've got [for treating alcoholism]." Needless to say, I was not as convinced and my blog drew some ire from one of the authors, who e-mailed me asking me to refrain from any more public comments and then posted their own response on the Nature wesbite (strangely through an intermediary!) Number 4: Strange Fruit: Is Racism a Mental Illness?
At Number 4 was my blog on whether racism could be a form of mental illness. Originally spurred by a newspaper article about a man who tried to use his schizophrenia diagnosis to mitigate his violent racist behaviour in court...and failed; and a subsequent Twitter interaction with @JonesNev, who argued that schizophrenia "often does lead otherwise liberal, kind, non-racist people to become glaringly,
bluntly racist, sexist, phobic, nymphomanic, hostile". Anyway, it led me to investigate past claims from psychiatrists that racism is an abnormal belief that could qualify as a delusion.
Number 3: CBT: She's Lost Control(s) Again
Number 3 was one of my several blogs about CBT. In this case, the first study to examine using CBT to alleviate symptoms in cases of psychosis where the individuals have chosen to be unmedicated. Of course, the study attracted wide media attention and for me, premature attention for their unfinished trial of CBT in unmedicated psychosis (e.g on BBC Radio 4 All in the Mind link in the blog). The study contains major methodological flaws, nobody should view it as other than fatally flawed and I await the results of their properly controlled trial for some interpretable data.
Number 2: CBT: You Spin me Round
At number 2, another CBT study and with the same main author as the unmedicated trial at number 3. This time it was using CBT to prevent transition to psychosis. The main upshot here is that it failed to show any effect - yet the authors went to extraordinary lengths to spin the results positively. We should not blame journalists when results are unreasonably/falsely represented in the media - however in this case: authors, media and even the journal (British Medical Journal) were at fault for spinning unanimously negative results
Number 1: Negativland: What to do about negative findings?
By a clear margin, my Negativland blog received the most hits. This post concerned the issue of how we deal with negative findings in science (psychology). Since this post, a great deal of much-needed discussion has occurred around this issue and about how psychology in particular might get its house in order. I have subsequently much expanded the ideas in this blog and hopefully, an article will appear in the Open Access journal BMC_Psychology in the New Year.
I have enjoyed my 10-month foray into blogging and much appreciate all of the feedback and interactions that have stemmed from this - thanks for your interest
Merry Xmas and a Happy New Year | |||
Saturday 22 December 2012
Santa Dog
Tuesday 11 December 2012
Significantly nonsignificant
In the morning I'd awake and I couldn't remember
What is love and what is hate? - the calculations error
What is love and what is hate? - the calculations error
Flaming Lips (Morning of the Magicians)
Cognitive behaviour therapy for psychosis can be adapted for minority ethnic groups: A randomised controlled trial
Shanaya Rathod, Peter Phiri, Scott Harris, Charlotte Underwood, Mahesh Thagadur, Uma Padmanabi & David Kingdon
Recently I have commented on what I see as methodologically poor, biased and spun studies of CBT for psychosis - every time I want to blog on someting else, out comes another questionable study - this time 'in press' at Schizophrenia Research, which I think requires comment - in particular, the gap between the reality and presentation of findings
This is an RCT looking at the use of CBT in UK minority groups with a diagnosis of schizophrenia
A total, n = 33 participants, who were randomly allocated to CBT for psychosis (CBTp n = 16) and treatment as usual (TAU n = 17). Although a relatively small study, the authors did a power analysis based on previous pilot studies and suggest that a minimum of 12 per arm of the trial would be sufficiently powered - obviously they exceed this expectation.
Did the CBT group show any benefit (i.e. reduction of symptoms) over the TAU group?
Well, the authors say yes in the abstract:
Results: Post-treatment, the intervention group showed statistically significant reductions in symptomatology on overall CPRS scores, CaCBTp Mean (SD) = 16.23 (10.77), TAU = 18.60 (14.84); p = 0.047,with a difference in change of 11.31 (95% CI:0. 14 to 22.49); Schizophrenia change: CaCBTp = 3.46 (3.37); TAU = 4.78 (5.33) diff 4.62 (95% CI: 0.68 to 9.17); p = 0.047 and positive symptoms (delusions; p = 0.035, and hallucinations; p = 0.056). At 6 months follow-up, MADRAS change = 5.6 (95% CI: 2.92 to 7.60); p < 0.001. Adjustment was made for age, gender and antipsychotic medication.
Conclusion: Participants in the CaCBTp group achieved statistically significant results post-treatment compared to those in the TAU group with some gains maintained at follow-up. High levels of satisfaction with the CaCBTp were reported
Flaming Lips - In the Morning of the Magicians
The key aspect here though is the bolded statement, added casually at the end of the results about 'adjustment'. Table 1 from the paper presented below indicates (as the authors rightly admit) that the TAU group were older, had longer duration of illness and greater medication and they duly adjusted analyses for these variables
Table 2 Results
Maybe someone can explain to me, what is happening here? Is it blatant author spinning to get further funding (as they mention this in the discussion). Is it collusion from reviewers, who let this through? Failure to spot the obvious by reviewers?
Perhaps I am overly critical - letters on a postcard (in the comments section please)
Monday 3 December 2012
Who Watches the Watchmen? Bias in Studying Bias
The coins are often very old by the time they reach the jeweller
With his hands and ashes he will try the best he can
He knows that he can only shine them
Cannot repair the scratches
With his hands and ashes he will try the best he can
He knows that he can only shine them
Cannot repair the scratches
The Jeweller (by Pearls Before Swine)
Publication bias in meta-analyses of the efficacy of psychotherapeutic interventions for schizophrenia.
Niemeyer & Musch & Pietrowsky (2012)
Niemeyer & Musch & Pietrowsky (2012)
Dan Dreiberg: I'm not the one still hiding behind a mask; Rorschach: No. You're hiding in plain sight. Interaction from The Watchmen
Hiding things in plain sight is often the best place to hide them! In my last blog, I referred to Daylight Robbery Syndrome where researchers say things so boldly that readers may be convinced of their validity even when they are not consistent with the data. Here I would like to refer to how researchers may intentionally or unintentionally hide something in front of the reader. In particular, how the application of methods used for detecting bias in meta-analyses may themselves be prone to their own biases.
This current paper, published recently in Schizophrenia Research, examines publication bias in studies of "psychotherapeutic interventions for schizophrenia".
Opening Scene from the Watchmen (Unforgettable by Nat King Cole)
As the authors Niemeyer et al rightly state:
"Meta-analyses are prone to publication bias, the problem of selective publication of studies with positive results. It is unclear whether the efficacy of psychotherapeutic interventions for schizophrenia is overestimated due to this problem. This study aims at enhancing the validity of the results of meta-analyses by investigating the degree and impact of publication bias."
This is certainly true for trials of psychological interventions, where the decision to submit a paper for publication is related to the outcome of the trial. For example, Coursol and Wagner (1986) found that when therapeutic studies had positive outcomes (i.e. clients improved) 82% submitted their paper, but with negative outcomes (client did not improve) only 43% submitted their articles (for similar conclusions from a recent meta analysis, see Hopewell et al 2009).
Returning to the current paper, Niemeyer et al used current standard meta-analytic methods to estimate bias, including: Begg and Mazumdar's adjusted rank correlation test, Egger's regression analysis and the trim and fill procedure. They applied these techniques to data sets derived from systematic reviews up to September 2010. I have remarked on these bias methods briefly in my previous post 'Negativland'.
Following their analyses Niemeyer et al concluded:
"Overall, we found only moderate evidence for the presence of publication bias. With one notable exception, the pattern of efficacy of psychotherapy for schizophrenia was not changed in the data sets in which publication bias was found. Several efficacious therapies exist, and their efficacy does not seem to be the result of publication bias."
This apparent lack of bias in this paper might be contrasted with the large bias documented by Cuipjers et al (2010) in studies examining CBT for depression. Cuipjers and colleagues found an effect size of .67 in 175 comparisons comparing CBT to a control condition; however adjustment for publication bias according to Duval & Tweedie’s trim and fill procedure reduced the mean effect size to 0.42 with 51 studies assumed to be missing i.e residing in file drawers because they were negative.
The Jeweler (by Pearls Before Swine)
I intend to concentrate briefly on the 10 data sets from meta-analyses for studies of CBT for schizophrenia (2 data sets from Lynch et al 2010; 1 from Lincoln et al 2008; 1 from Wykes et al 2008; 5 from Zimmerman et al 2005; and 1 from Jones et al 2010: see Table 1)
Table 1. Bias analysis of CBT for schizophrenia meta analyses (from Niemeyer & Musch 2012)
1) Our meta analysis (Lynch, Laws & McKenna 2010) criticised for being overly selective by some (because we analysed high quality studies using an active control group!) produced a data set with the fewest imputed (i.e. missing studies)
2) The Wykes et al (2008) analysis is curious. First the authors state that the effect size was Cohen's d - when in fact Glass' delta was used (a quite different effect size). This could of course be a simple error. The choice of outcome variable, however, is not an error - the authors chose to analyse Low Quality studies from the Wykes paper. Why would a study of bias select only low quality studies and not the high quality or at least both?
Table 2 shows where these (positive symptom) effect sizes were derived from the Wykes et al paper. What is clear is that the low quality studies are not significantly heterogeneous, while the high quality studies show significant heterogeneity - indeed this is partly borne out by the far broader spread of scores for the 95% confidence intervals in high quality studies (even though they constitute almost half the number of low quality studies)
Table 2 Effect sizes from Wykes et al (2008)
By selecting low quality studies, it would seem that the probability of finding bias may be diminished and at the very least, the estimate of bias is unreliable
3) From the Lincoln et al (2008) meta-analysis, the authors selected data for 9 studies comparing CBT vs TAU. Omitted, however, was an additional comparison of 10 studies of CBT vs active control (see Table 3 below)
Table 3. Data from Lincoln et al (2008) Meta-analysis
The notable thing again is that the authors chose to exclude one analysis that has: a) a larger sample b) a non-significant effect and c) far greater 95% Confidence Intervals i.e. variance. Again, these factors could obviously conspire against finding bias and leave us uncertain about bias in this meta-analysis.
4) From the Zimmerman et al meta analysis, the authors included 5 analyses and all bar the last had proportionally large numbers of imputed studies. The one comparison that produced no imputed studies was the comparison with an 'active' control (like Lynch et al - which also produced no imputed studies)
5) Finally Niemeyer & Musch selected one comparison from the Jones et al (2010) Cochrane meta-analysis - a somewhat odd choice to be included - measuring 'relative risk for leaving a study early'.
These decisions are made somewhat odder and less reliable by the fact that Niemeyer & Musch failed to include any data from meta-analyses by the same Cochrane group examining symptoms (Jones et al 2004) or indeed other meta-analyses such as that by Rector and Beck (2002) or the UK NICE Committee (2009)
Anyway, to conclude, the bias analysis of CBT for Psychosis by Niemeyer et al is itself biased by unexplained choices made by the reviewers themselves. Not being psychic, I have no idea why they made these choices or what differences it would make to include different measures and additional meta-analyses. One thing I do know, however, is that any claim that bias does not exist in studies examining CBT for psychosis...is a biased and unreliable! Researchers are familiar with the idea of GIGO (Garbage In Garbage Out), which has often been levied at meta-analysis - perhaps we now need to consider METAGIGO!
3) From the Lincoln et al (2008) meta-analysis, the authors selected data for 9 studies comparing CBT vs TAU. Omitted, however, was an additional comparison of 10 studies of CBT vs active control (see Table 3 below)
Table 3. Data from Lincoln et al (2008) Meta-analysis
The notable thing again is that the authors chose to exclude one analysis that has: a) a larger sample b) a non-significant effect and c) far greater 95% Confidence Intervals i.e. variance. Again, these factors could obviously conspire against finding bias and leave us uncertain about bias in this meta-analysis.
4) From the Zimmerman et al meta analysis, the authors included 5 analyses and all bar the last had proportionally large numbers of imputed studies. The one comparison that produced no imputed studies was the comparison with an 'active' control (like Lynch et al - which also produced no imputed studies)
5) Finally Niemeyer & Musch selected one comparison from the Jones et al (2010) Cochrane meta-analysis - a somewhat odd choice to be included - measuring 'relative risk for leaving a study early'.
These decisions are made somewhat odder and less reliable by the fact that Niemeyer & Musch failed to include any data from meta-analyses by the same Cochrane group examining symptoms (Jones et al 2004) or indeed other meta-analyses such as that by Rector and Beck (2002) or the UK NICE Committee (2009)
Anyway, to conclude, the bias analysis of CBT for Psychosis by Niemeyer et al is itself biased by unexplained choices made by the reviewers themselves. Not being psychic, I have no idea why they made these choices or what differences it would make to include different measures and additional meta-analyses. One thing I do know, however, is that any claim that bias does not exist in studies examining CBT for psychosis...is a biased and unreliable! Researchers are familiar with the idea of GIGO (Garbage In Garbage Out), which has often been levied at meta-analysis - perhaps we now need to consider METAGIGO!
Tuesday 27 November 2012
In a Manner of Speaking
In a Manner of speaking
I just want to say
That I could never forget the way
You told me everything
By saying nothing
I just want to say
That I could never forget the way
You told me everything
By saying nothing
In a Manner of Speaking (by Tuxedo Moon)
I was recently asked to write an article on some of the problems associated with psychological research (e.g. publication bias, authors 'spinning' their results and so on). We often hear complaints from scientists that journalists put a false spin on their findings; however, I am interested in how authors present or spin their own findings.
Sometimes this spinning in a paper seems to starkly contrast with results of the paper. I can only conclude that some reviewers or editors suffer from what I would call the 'Daylight Robbery Syndrome' - from the adage that some burlgars are unlikey to be caught because they rob you so blatantly. Here are my current top five quotes from papers on CBT for psychosis published in high impact journals ...For me, the quotes are the academic equivalent of someone kicking down your front door in broad daylight and then carrying off your 42 inch plasma TV screen under their arm past all of your friends and neighbours...
Sometimes this spinning in a paper seems to starkly contrast with results of the paper. I can only conclude that some reviewers or editors suffer from what I would call the 'Daylight Robbery Syndrome' - from the adage that some burlgars are unlikey to be caught because they rob you so blatantly. Here are my current top five quotes from papers on CBT for psychosis published in high impact journals ...For me, the quotes are the academic equivalent of someone kicking down your front door in broad daylight and then carrying off your 42 inch plasma TV screen under their arm past all of your friends and neighbours...
Therapeutic work is rife with vague statements, bias and misrepresentations; however, I am sure comparable examples exist in other areas and that readers may readily be able quote examples from their own research areas.
The editorial goes on to discuss the largest, best and most recent study of art therapy for addressing the symptoms of people with schizophrenia (the so-called Matisse trial by Crawford et al 2012)
1. " Interestingly, psychosocial treatments—such as cognitive behavioural therapy (CBT) and, more recently, arts therapies (music therapy, art therapy, and body movement or dance therapy)—have shown more promise than drug treatments in reducing negative symptoms and their impact, and the National Institute for Health and Clinical Excellence (NICE) has recently recommended these treatments."
"The findings of the Matisse trial unfortunately suggest that art therapy, as currently practised in the UK, is unlikely to be of clinical benefit for people with negative or other symptoms of schizophrenia—a conclusion that the profession of art therapy will no doubt find unsettling. However, arts therapies, because they rely on creative expression rather than verbal communication, and some cognitive behavioural approaches, still have the greatest potential for success in the treatment of negative symptoms."Kendall, T. (2012). Treating negative symptoms of schizophrenia. BMJ-British Medical Journal, 344(7847), 8.
In additon to the elephantine self-contradiction of the latter paragraph - two other things are wrong here. First, CBT does not significantly reduce negative symptoms - Wykes et al (2008) meta-analysis shows that studies with "acceptable" levels of quality find no significant impact of CBT on negative symptoms. Second arts therapy does not appear to reduce psychotic symptoms nor does it outperform medication in reducing negative symptoms. The fact is that no study has compared medication versus any of these therapies ...and so, no data even exist on the issue.
Perhaps Editorials - unlike this one in the BMJ - really ought to be peer-reviewed!
2. Although we failed to show a statistically significant effect of the intervention we cannot rule out a beneficial effect of the cognitive therapy on transition rate (although it could be argued that the sample size required to show such an effect, and the small effect sizes reported here, would make such an endeavour unfeasible in practical terms and unwarranted in clinical terms).Morrison AP, Stewart SL, French P, Bentall RP, Birchwood M, Byrne R, Davies LM, Fowler D, Gumley AI, Jones PB, Lewis SW, Murray GK, Patterson P, Dunn G. Early detection and intervention evaluation for people at risk of psychosis: multisite randomised controlled trial. British Medical Journal, 344
The failure to find a significant effect does not eliminate possibility of an effect! I have to ask, what could then eliminate the possibility of an effect...especially with a very small effect size and a huge sample required? Extremely torturous admission of CBT failure...or is it?
3. Patients receiving either CBT or supportive counselling in combination with usual treatment demonstrated better symptomatic recovery but no significant reduction in relapse compared with those receiving usual treatment alone... We suggest that the optimum psychosocial management of early schizophrenia would include a combination of CBT and family intervention.
Tarrier, N., Lewis, S., Haddock, G., Bentall, R., Drake, R., Kinderman, P., ... & Dunn, G. (2004). Cognitive-behavioural therapy in first-episode and early schizophrenia 18-month follow-up of a randomised controlled trial. The British Journal of Psychiatry, 184(3), 231-239.
How to ignore one whole strand of the main findings and also to make a nonsignificant result sound as if it were significant! CBT was no better than Supportive Counselling and yet the authors advocate CBT alongside family intervention - and the latter was not examined at all in this study...a strange conclusion-cocktail!
4. We did not find significant between-group differences on symptom reduction, indicating no significant benefit of CBT over PE.” [psycho-education]...The use of an active rather than passive control intervention created a more stringent comparison for CBT, which may have further reduced power to detect the hypothesized changes”
Cather, C., Penn, D., Otto, M. W., Yovel, I., Mueser, K. T., & Goff, D. C. (2005). A pilot study of functional cognitive behavioral therapy (fCBT) for schizophrenia. Schizophrenia Research, 74(2), 201-209.
The finding of no significant benefit of CBT is blamed on a pesky control group - those cheeky controls reducing power! If only we hadn't used controls, our results, we would have had a significant result .. hey diddle diddle...
5. In the linear regression, faster resolution of symptoms in the groups allocated to either psychological treatment condition was seen, compared with routine care alone, but not at statistically significant levels...In summary, for auditory hallucinations, CBT is an improvement on routine care (but the effect is not statistically significant at the α =0.05 level)
Lewis, S., Tarrier, N., Haddock, G., Bentall, R., Kinderman, P., Kingdon, D., ... & Dunn, G. (2002). Randomised controlled trial of cognitive—behavioural therapy in early schizophrenia: acute-phase outcomes. The British Journal of Psychiatry, 181(43), s91-s97.
It doesn't mater how many times one says 'faster', 'better', improvement' - 'No'significant effect' means no significant effect!
Blind commitment to a theory is not an intellectual virtue: it is an intellectual crime.
Imre Lakatos (1970)
Sunday 11 November 2012
CBT: She's Lost Control(s) Again
And of a voice that told her when and where to act,
She said I've lost
control again
She said I've lost
control again
Joy Division (Shes Lost Control Again)
Cognitive therapy for people with a schizophrenia spectrum diagnosis not taking antipsychotic medication: an exploratory trial
Morrison, Hutton, Spencer, Barratt, Brabban, Callcott, Christodoulides, Dudley, French, Lunley, Tai & Turkington
This study, published recently in Psychological Medicine marks a departure from previous CBT for psychosis studies as it involves administering CBT to individuals who are unmedicated - and alongside the media attention (All in the Mind), it is important to look more closely at the study itself.
Morrison and 11 colleagues examined a small sample of 20 participants with schizophrenia spectrum disorders (actually 18 and one also didn't complete the therapy - so 17). All were outpatients - who had not been taking antipsychotic medication for at least 6 months. Morrison et al measured the impact of CBT on symptomatic outcome measures: Positive and Negative Syndromes Scale (PANSS), which was administered at baseline, 9 months (end of treatment) and 15 months (follow-up). Secondary outcomes were dimensions of hallucinations and delusions, self-rated recovery and social functioning. Rather than dismiss missing data, the authors chose to impute the missing data in the following analyses:
Their main findings were stated as:
"significant beneficial effects on all primary and secondary outcomes at end of treatment and follow-up, with the exception of self-rated recovery at end of treatment. Cohen’s d effect sizes were moderate to large [for PANSS total, d=0.85, 95% confidence interval (CI) 0.32–1.35 at end of treatment; d=1.26, 95% CI 0.66–1.84 at follow-up]."
The authors conclude that the
"study provides preliminary evidence that CT is an acceptable and effective treatment for people with psychosis who choose not to take antipsychotic medication. An adequately powered randomized controlled trial is warranted."
Now, I do think this is important because some individuals may see this study and attendant media as a basis to decide not to take antipsychotic medication. I have no qualms about personal choice when based on evidence - so let us examine the evidence.
Joy Division: Shes Lost Control
So, what does the study show? Well, the answer comes from the design of the study. It is a pretest - posttest design i.e. there is no control group. So, a within-group analysis with no control group. Without a control group of any description, we cannot know if any change is a generalised consequence of the added interaction (rather than anything about CBT itself). And without even a Treatment as Usual (TAU) control group, we cannot exclude the possibility that any change would have occurred regardless of therapy e.g. regression to the mean.
Second, the trial is an Open Trial i.e. the outcome measures are not made blind. All participants are evaluated by members of the team who were involved in the administering the trial. The lack of blinding is the biggest drawback to the evaluation of therapy and is well documented by all meta-analyses in this area (Lynch, Laws & McKenna 2010; Wykes et al 2008).
So, the study suffers from a host of threats to validity: a) regression to the mean i.e. extreme scores at start simply move toward the (lower) mean on second testing (with no control we cant estimate or eliminate this); b) Hawthorne effect i.e. any change is due to the special circumstances patients find themselves in (with no control, we cant eliminate this); c) lack of blinding i.e. those measuring outcome were involved in the study and aware that all patients had received CBT - the authors don't provide detail on this, but presumably some or all of the 8 different therapists administering the CBT to the participants and/or those who designed the study
Losing Control adds up!

To summarise - no control group and no blinding of outcome measures.
Can we see what happens in such designs with medicated patients? Well, below is a table from a meta-analysis by the CBT guru Aaron Beck looking at effect size for pretes-posttest analyses in medicated patients (Rector & Beck 2002; so 'good' the journal republished it in 2012). Now Morrison et al found d=.85 for overall symptoms -Rector and Beck report a much larger mean effect size of d=1.31 for pre-post comparison (CBT-RC). So, the effect with unmedicated is substantially less - consider the size in some studies here - Pinto is almost three times that reported by Morrison et al!
This doesn't alter the fact that Morrison et al do report a substantial effect in unmedicated patients of .8+. However, the second thing to note about the table above is the comparison of CBT with a so-called active control (ST-RC) i.e. a condition that controls for the generalised impact of just interacting with another, receiving attention etc - here the controls are supportive therapy, befriending and so on. This shows that an effect size of .63 emerges in pretest postest designs for something as simple as befriending - not that much smaller than Morrison et al claim to attribute to CBT.
The final and key point though concerns the lack of blind evaluation. As Morrison et al note in their discussion:
"CBT for psychosis trials that attempt masking were reported to be associated with a reduction of effect sizes of nearly 60% (Wykes et al 2008)"
Actually, what Wykes et al say is
"There is a tendency for the unmasked studies to be overoptimistic about the effects of CBTp, with effect sizes of 50%–100% higher than those found in masked studies."
60% may be an average, but the reduction could range from 50-100%!
Crucially, the patients may not feel better. At the end of the study, the patients rated themselves as experiencing no recovery (pre and post); although they did report a minor improvement at the follow-up. In other words, the non-blind researchers perceived a much greater change than the patients themselves - approximately double the effect size!
To conclude: the use of a pretest-posttest design with no blinding means the authors are unable to draw conclusions about the efficacy of CBT in the study. The effect size is much smaller than in pretest-postest comparisons with medicated patients; of the .85 reported, how much is attributable to generic effects of interaction (and nothing to do with CBT) - well it could be .63; and if we assume a minimum of 60% of this may reflect lack of blinding - then what are we left with? An effect size of possibly less than .1 - in other words - (next to) nothing! And patients are not even convinced!
So, their conclusions that the "study provides preliminary evidence that CT is an acceptable and effective treatment for people with psychosis who choose not to take antipsychotic medication" seems unwarranted. Some might say, well its called 'exploratory' - but that is no excuse for a design that leaves the data uninterpretable and may even lead to some people changing their behaviour (withdrawing from their medication). I also understand that an RCT with blind assessment is being conducted - indeed, much of the press around this study has been about the uncompleted study - a bit cart before the horse! But at the moment - no data published exist to show that CBT reduces psychotic symptoms in unmedicated individuals
References
Lynch, D., Laws, K. R., & McKenna, P. J.
(2010). Cognitive behavioural therapy for major psychiatric disorder: does it
really work? A meta-analytical review of well-controlled trials. Psychological
medicine, 40(01), 9-24.
Wykes,
T., Steel, C., Everitt, B., & Tarrier, N. (2008). Cognitive behavior
therapy for schizophrenia: effect sizes, clinical models, and methodological
rigor. Schizophrenia Bulletin, 34(3), 523-537.
Wednesday 19 September 2012
Drug Buddy: Ecstasy to self-medicate depression?
This is not ecstasy, but it's better than cocaine.
and you know that I will miss you when you're gone
but I'm not equipped to play this game
The Czars (Drug)
and you know that I will miss you when you're gone
but I'm not equipped to play this game
The Czars (Drug)
by Majumder, White & Irvine (in press) Addictive Behaviours
Majumder et al look at the topical and fascinating notion that people with a pre-existing mood disturbance may be using ecstasy as a ‘self-medication’. Given recent media reports about possibly using of MDMA to treat depression and the Channel 4 TV show Drugs Live: The Ecstasy Trial ...although presented by the media as looking at MDMA for depression, it seems to be more traumatic memories (but we haven't seen the show yet!)
does this short report of Majumder et al get us rolling...?
What did Majumder et al do? They compared the immediate effects of ecstasy on mood in subjects divided into those with (WP) and without (NP) a predisposition to depression (as assessed using the Brief Symptom Inventory: BSI) before and after a 'party'.
65% of the NP group were females, whereas in the WP group the male to female ratio was 2:1 (χ2(1)=4.912, p=0.027). The authors say "Other demographic parameters were similar between the groups [and]...No significant differences were observed between groups for ecstasy use or recent use of other substances (though details are missing)
65% of the NP group were females, whereas in the WP group the male to female ratio was 2:1 (χ2(1)=4.912, p=0.027). The authors say "Other demographic parameters were similar between the groups [and]...No significant differences were observed between groups for ecstasy use or recent use of other substances (though details are missing)
The Czars (Drug)
Method
The baseline session was scheduled when participants were drug free (confirmed by a urine test) for at least 7 days prior. All subjects were asked to fill out three self-assessment questionnaires: the Brief Symptom Inventory (BSI), the Beck Depression Inventory (BDI) and the Profile of Mood States (POMS).All participants were invited to attend a "party session" (and details about this are sketchy e.g. were they were all together - which could influence who does and doesn't decide to take the Es); and crucially, we assume they arrive with their own Es - however many?)
Participants were assigned to either the ecstasy or control group "based on their intention to consume a pill during the social gathering." The authors state "There was no encouragement to consume a pill for the purposes of the study. Subjects in the ecstasy group notified the investigator when they consumed a pill via text message, and 60min later the investigator administered the BDI and POMS by telephone and asked participants to provide a saliva sample in a plastic tube given to them prior to the party session."
The Lemonheads (My Drug Buddy)
Results
(All variance measures are SE). During the social gathering, the NP group reported consuming average of 1.7±0.33 pills, and those in the WP group 1.4±0.22 pills (not significantly different).
The mean MDMA concentration in saliva was 896±132.1 ng/ml (n=17). Crucially, again some detail is missing - they don't give MDMA concentration for the two separate groups, but for whole group. Urine screening tests the following day confirmed exposure to MDMA of subjects in the ecstasy group and did not detect MDMA in any of the control group samples. Other substances consumed were alcohol, cannabis and tobacco, but no difference was observed between the groups.
As expected, when drug-free, the WP subjects show greater mood disturbance and depressive symptoms than the NP group (POMS: NP 5.85±1.63, WP 14.5±2.81, p<0.05, BDI: NP 4.9±0.86, WP 11.2±1.65, p<0.01). Turning to the main reuslts:
Beck Depression Inventory (BDI) The authors report that "During social gathering, WP subjects who consumed ecstasy reported a significant decrease in depressive symptoms (F(1,35)=5.47, p<0.05). We can see this reduction in bottom figure (b).
However, the authors fail to say anything about the top left figure (a) - where the No Predisposition group show far greater depression (BDI scores) than controls after taking ecstasy - this looks, if anything, a larger difference than the purported reduction (after E); and even a reduction in depression symptoms for the controls themselves who don't take E (which seems as quite large given the small SE bars)
Profile of Mood States (POMS)
POMS: No significant effect of E on mood emerged. The authors state "No interaction or main effects of the drug group and predisposition to depression scores at the party session were observed."
This seems slightly odd given that every group showed a reduction of POMS scores (see Figure below) whether they had predispotion or not, took E or not!
Conclusions
The authors conclude "A decrease in depressive symptoms was observed in subjects predisposed to depression. This antidepressant-like action of MDMA may contribute to its use, particularly among people with an existing or latent depressive disorder."
To me it seems a few questions remain:
1) Did the participants take E together? what are the consequences of social desirability and bravado?
2) Why was the MDMA concentration not given for separate groups (WP and NP) who took E? This is important information as we dont know what the WP and NP groups took
3) Did the BDI scores of controls decrease significantly in the NP condition?
4) In the NP condition, do the E users show significantly greater BDI scores than controls at the party?
5) If BDI does decrease, why is POMS left unaffected? or is it unaffected given all groups show a reduction, why is the main effect for before and after party not sigificant (possibly a lack of power?)
Monday 10 September 2012
Come Sta La Luna: fingernails and depression
I saw it written and I saw it say
Pink moon is on it's way
And none of you stand so tall
Pink moon gonna get you all
It's a pink moon
Hey, it's a pink moon
Nick Drake (Pink Moon)
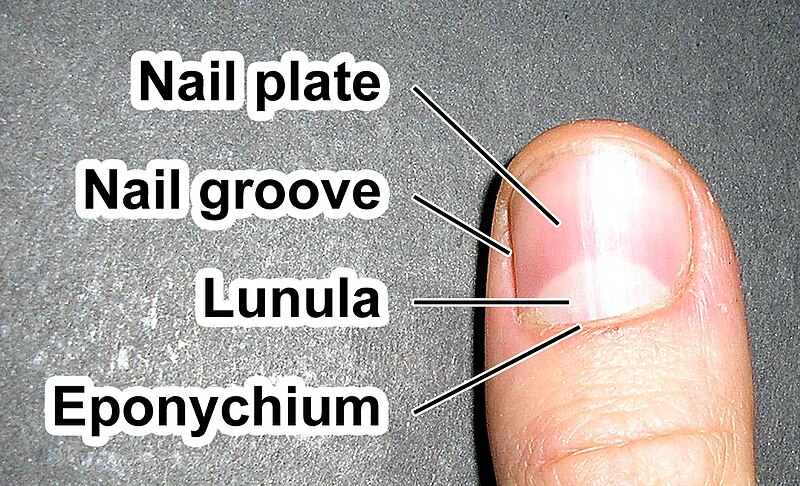
Psychiatry Research has just published a somewhat leftfield paper about fingernails and depression by a group of Chinese scientists. The association between absent lunula and depression in depressive outpatients: A case-control study by Zhou et al (2012). It concerns the lunula (Latin Little Moon), which is the white, half-moon shape often visible on all fingers except the little finger.
Absent lunula are apparently associated with various systemic disorders including hypopituitarism, hypothyroidism, iron deficiency anaemia, arteriosclerosis, malnutrition, chronic renal failure, and even cancer (e.g. Cohen, 1996).
Zhou et al state that in "Traditional Chinese Medicine absent Lanula are associated with lower physiological response and bad microcircualtion" and then use this as leverage for hypothesising that absent lunula may be linked to depression.
Present Lunula Absent Lunula


The authors examined fingernails in a large sample of 332 depressive outpatients (aged between 19 and 67) without cutaneous, congenital or other systemic diseases; and without application of drug and henna that might contribute to any change of lunula. They compared the patients with a similarly large sample of 367 healthy controls, who were drawn from ‘spouses of the patients’ or local residents. The two groups were well matched for age and sex.

Whose nails are they ...was he depressed? Not mine! (but belong to someone well-known at least to UK public)
Come Sta La Luna (by Can) - if feeling unwell, the cure is in the Can
The Zung Self rating Depression Scale (ZSDS: Zung, 1965) was used to measure the level of depression with scores of <50 =normal; 50–59=mild depression; 60–69=moderate depression; and 70=severe depression (Lin et al., 2009).
Then they simply observed for absence of luluna on right hand (as right and left tend to be identical in this respect). People were classified as having 1,2, 3 or no luluna (as noted the little finger is excluded having no lunula anyway)
Pink Moon (by Nick Drake) followed by the Black Dog
A large difference emerged with only 17.2% of depressed having all 4 lunula present compared to 68.1% of controls. At the other end, 23.7% of the depressed group and only 9.8 of controls had 4 missing (see Table 2)
Table 3 compares absent lunula in relation to depression severity within the depressed group. The table show no differences in sex and age composition between mild/moderate vs severely depressed but that 69% of severe depressed have >3 absent lunula while in the mild/moderate depressed this figure is 41.7%.
Conclusion - mechanism?
The authors state that
"Though the mechanism of absent lunula is still not clear and disputed, previous researches [sic] agreed that absent lunula reflects a variety of complex factors including metabolic changes in addition to anaemia (Dyachenko et al., 2007;Salem et al., 2008;Saray et al., 2004). Metabolic changes are also included in the mechanism of depression, such as the metabolic disorders of angiotensin-converting enzyme, serotonin, monoamine, cortisol, brain-derived neurotrophic factor, melatonin and so on (Akpinar et al., 2008; Annerbrink et al., 2010; Belmaker and Agam, 2008; Montag et al., 2010; Okuno et al., 2011; Wang et al., 2009). Therefore, it may be possible that absent lunula and depression have a common metabolic process leading to the co-occurrence of them."
While the explanation is somewhat speculative and opaque, it is an intriguing finding showing that a small visible finger detail (lunula) may provide information about inner mental state. Looking at my own fingers, my two hands are quite different - lateralised depression! Perhaps a link between mental health and the 'Moon' has some basis after all, but in a positive manner ...check for your good Moon rising...

Whose nails are they ...was he depressed? Not mine! (but belong to someone well-known at least to UK public)
Thursday 6 September 2012
Strange Fruit: Is Racism a Mental Illness?
The weakest link in every chain
I always want to find it
The strongest words in each belief
Find out what's behind it
Politics is pride too
Vagaries of science
She left because she understood
The value of defiance
I always want to find it
The strongest words in each belief
Find out what's behind it
Politics is pride too
Vagaries of science
She left because she understood
The value of defiance
Scritti Politti (The Sweetest Girl)
Recently I came across a, sadly, all too common newspaper article about racism in the UK - the story concerned a man (Mr Swift) found guilty of racially abusing staff at his local shop. The 32 year-old man racially abused two staff, made Nazi salutes, called a woman in the shop a "black ****" and said "go back to your country you bitch".
What made this story marginally more interesting was that the man's defendant Paul Morris said "Swift suffers from schizophrenia and part of his behaviour in recent years has been a direct result of the illness" - he claimed, or at least implied (given the way that Lawyers use language), that the racism was somehow linked to his schizophrenia
On reading the article, I tweeted “Astonishing – Defence claims schizophrenia caused man to be aggressive racist twat.” And within a couple of hours, I received a tweet from @JonesNev linking me to her interesting Ruminations on Madness blog, where she articulated a thought-provoking (albeit ambivalent) retort to my tweet - it is called 'Culture and Delusions'
In the blog, Nev says:
Although I’m not entirely comfortable with my apparent self-appointed role as apologist for (schizophrenic) mass shooters and racists, it seems necessary to underscore the extent to which severe psychosis in fact can and often does lead otherwise liberal, kind, non-racist people to become glaringly, bluntly racist, sexist, phobic, nymphomanic, hostile, anti-Semitic and so on. I struggle to articulate this in a way that does not directly equate psychosis with pathology, but it seems relatively unambiguous that, at least in some cases, the dynamic “re-mixing” of (emotionally charged) cultural motifs with personal (conscious and/or unconscious) fears and insecurities, profound experiential changes in the boundaries between self and other, disorganization and slippage of thought and memory, sometimes bizarre and frightening voices and visions, often very unsurprisingly leads to a kind of unwitting and strangely cultural “performance” of otherwise more broadly salient sociopolitical conflicts. (And what, of course, is more culturally salient than race?) One might also speculate that implicit racism (which virtually all of us tacitly endorse, as social psychologists have repeatedly demonstrated) simply boils to the surface in the cauldron of psychosis."
Could racism result from delusional thinking?
Nev's response got me thinking - could schizophrenia or a delusional state really cause a person, who was hitherto not racist... to become a violent or abusive racist?
But I have worked for 20+ years with many deluded individuals - some claiming to be John Lennon, the Queen's son, or even Green Gartside, but unlike Nev I have yet to meet one who changed from being a non-racist to an aggressive racist following their 'illness'. I have, of course, encountered some expressing politically incorrect views, but none who radically changed! While psychosis can produce dramatic transformations large enough to impact personal identity, as far as I can determine empirical data are sadly lacking on radical transformation of sociopolitical beliefs in psychosis.
Jacques Derrida is in love with Green Gartside
Are we all racists under the surface?
What about the notion that racism is implicitly bubbling under the surface in most or all of us? Evidence used to underpin this idea comes from the Implicit Association Test - but I don't think it holds much water. I don't doubt that the IAT (test yourself here) reveals some associations may occur faster than others - what I object to is the notion that such associations signify racism (implicit or otherwise). Little or no evidence exists to document a link between IAT performance and overt discrimination. And a recent meta-analysis (Greenwald et al. 2009) found a very small association between performance on the Race (black-white) IAT and explicit (self-report) measures in 27 studies (with an r=.11). The bottom line is little or no evidence for a link between the IAT with overt racism; and of course, if most of use show implicit racism, why do only a fraction become overt racist? If only we could cure racism with propranolol...
Defining delusions
Could racist behaviour qualify as delusional? According to the DSM-IV-TR, a delusion is:
A false belief based on incorrect inference about external reality that is firmly sustained despite what almost everybody else believes and despite what constitutes incontrovertible and obvious proof or evidence to the contrary. The belief is not one ordinarily accepted by other members of the person's culture or subculture.
Does racism meet the criteria for being a delusion? Yes...racism could be a false belief based on incorrect inference about external reality and one that is not one ordinarily accepted by other members of the person's culture.
In the case of Mr Swift, I think the correspondence may lack when we consider "firmly sustained despite what almost everybody else believes and despite what constitutes incontrovertible and obvious proof or evidence to the contrary" Interestingly, in interview, Swift told police officers he remembered swearing and telling the shopkeepers to get out of his country, but he was not racist. Now, without being too picky (and leaving absurd "some of my best friends are black' reverse psychology nonsense), some might argue that his denial of being a racist undermines the claim about it being delusional. If only we could get deluded individuals to so readily give up their delusions (as perhaps a legal defence team), then I suspect we might dispense far less medication or psychological therapy!
As an aside, the person who thought they were Green Gartside looked nothing like him, being much heavier, shorter and with red hair - when I pointed out the inconsistency, he informed me that the hospital had cut parts of his legs away and given him chemicals to change his hair colour and make him partly bald - invention and resistance are key to the survival of delusion!
If music could cure racists (a memory from my youth 30/4/1978)
Racism as a form of mental illness: Alvin Poussaint
Some within psychiatry, notably Harvard University psychiatrist Alvin Poussaint have argued that racism itself should be recognised as a mental illness. In a New York Times article entitled "They Hate. They Kill. Are they Insane?" in 1999, he argued that:
It is time for the American Psychiatric Association to designate extreme racism as a mental health problem. Clinicians need guidelines for recognizing delusional racism in all its stages so that they can provide treatment. Otherwise, racists will continue to fall through the cracks of the mental health system, and we can expect more of them to act out their deadly delusionsIn another article entitled 'Is extreme racism a mental illness" Poussaint argues that:
To continue perceiving extreme racism as normative and not pathologic is to lend it legitimacy. Clearly, anyone who scapegoats a whole group of people and seeks to eliminate them to resolve his or her internal conflicts meets criteria for a delusional disorder, a major psychiatric illnessHowever, he also claims that common or garden varieties of racism are treatable:
"...sometimes even lesser forms of racism are treatable because they have psychodynamics to them...They don't exist as a social problem, they … exist as psychological problems inside the individual."In a piece in the Western Journal of Medicine Poussaint proposes specific modifications to the DSM’s diagnostic criteria for delusional disorder, suggesting the prejudice subtype:
A delusion whose theme is that a group of individuals, who share a defining characteristic, in one’s environment have a particular and unusual significance. These delusions are usually of a negative or pejorative nature, but also may be grandiose in content. When these delusions are extreme, the person may act out by attempting to harm, and even murder, members of the despised group(s).Poussaint makes some valid arguments, but the dilemma we are faced with is...arent most violent hate crimes largely committed by people who are bad, not mad?
You needn't take it any further, sir. You've proved to me that all this ultraviolence and killing is wrong, wrong, and terribly wrong. I've learned me lesson, sir. I've seen now what I've never seen before. I'm cured! Praise Bog! I'm cured!
Alex (Clockwork Orange)
References
Douglas, K., Guy, L., & Hart, S. (2009). Psychosis as a risk factor for violence to others: A meta analysis. Psychological Bulletin, 135, 679–706.
Fazel S, Gulati G, Linsell L, Geddes JR, Grann M (2009) Schizophrenia and violence: systematic review and metaanalysis. PLoS Med 6(8):1–15
Greenwald, A. G., Poehlman, T. A., Uhlmann, E. L., & Banaji, M. R. (2009). Understanding and using the Implicit Association Test: III. Meta–analysis of predictive validity. Journal of Personality and Social Psychology, 1, 17–41.
Subscribe to:
Posts (Atom)